This quarantine for COVID-19 is something to ponder especially for those in a clinical setting!
I’m afraid the numbers who are suffering from Covid-19 may scare you too much especially when there's nothing else to think about, so I hope my cooking posts help take your mind off of it!!!

In 2016, I was in London, England in support of a distant uncle that is facing his last battle with metastatic colon cancer, who had just undergone a major bowel resection. He has woken up since and verbalized he wanted every medical procedure done to keep him alive, but there was a period of uncertainty of whether he was going to make it through the night. We were his only family there that was expected to decide if the medical team was to try everything they could to save his life. I reflected back to when I was working as a clinical dietitian…
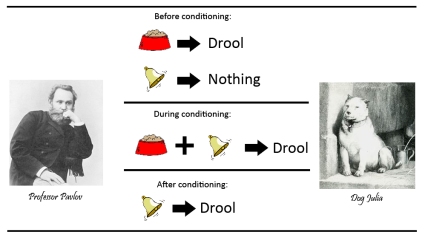
I remember working on my residency at one of the most prestigious cancer centers in New York City as a dietetic intern and how many times a week I heard, “Let’s help with that family’s decision with a patient’s DNR/DNI consent,” when the patient was lying either unconscious or unable to make his or her own medical decisions — It was ultimately up to the family/healthcare proxy. As a part of the medical team, I was there to decrease the amount of pain and provide the most comfortable situation for my patient. I felt like Pavlov’s Dog, conditioned to think that the DNI/DNR order was the ticket to a show, watching someone live his or her life to the end enjoying the concoction of painkillers with a warm glass of milk while sitting on a rocking chair next to the fire place. In many cases patients could not even eat or swallow anymore and I was the one who calculated the patient’s tube feeding to support their daily nutritional needs. “Comfort” was essentially the goal of the medical plan of palliative care and we were trained to think that that was the right thing to help a cancer patient at the last stages of disease, unable to verbalize his own choice.
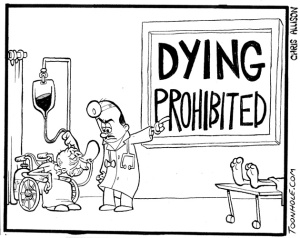
Well, being in a different pair of shoes there in London, I was undecided as to whether or not the notion of “comfort,” was entirely clear. Sure, quality of life was important, but to a vulnerable person who was not ready to face death, their idea of dying slowly without a fight, may not be a wholesomely “comfortable” idea to them –This is the dilemma. What does “comfort” really mean? …Who was really made comfortable here? The family or the patient?
I asked one of my best friends whether my uncle should be intubated or not at this point. She is an anesthesiologist who is practicing at one of the most well known teaching hospitals in the world, and she said, “... the option is dying with the tube Or dying without the tube” –I was left to interpret that myself… When I was a clinician, that message would have been crystal clear, but now, it just put a bigger hole in my chest. I love her to death and I do not think she was coldhearted to any extent by saying that, she is a doctor and it was what was delivered for the patient’s best interest, but that really made me think.

I recently saw the play, “Tuesdays with Morrie” by Mitch Albom. A very touching story about a professor, Morrie Schwartz, battling his illness with ALS , an incurable progressive neurological disease. It really made me reflect on how many times I took my life for granted and how many times I took other people’s lives for granted. It was a very emotional 2 hours of my life which, helped me understand some things about being human.
Not everything is black and white, just like the DNR/DNI consent will never be a concrete order to me anymore. Kudos to those who work at a hospital and face such decisions in their daily life, I applaud you.
I am no longer practicing clinically in hospitals or care homes, but instead I am taking the preventative role. I want to prevent disease before it is diagnosed and I want to see people who want to make a change in their lifestyles take their lives back in their own hands. In the end, nobody should be put in the spot to make the decision to “do not resuscitate or do not intubate” for anyone else, but themselves!
So, I’m really only here for the food! 🙂 In the end, I’d much rather prescribe something you can see, chew, and swallow rather than something that goes through a tube that is not so appealing to eat!

Going back to the subject of Covid-19, keep your family and friends safe out there, we are all in this together!!! Prayers and thoughts to those who are on the frontline in the pandemic!
Written By: Renée Y. Chan, MS, RD, Founder of True NOSH
Registered Dietitian